9am-5pm, Mon - Fri excludes Bank Holidays.
8am-5pm, Mon-Fri excludes Bank Holidays.
Open 24 hours, 7 days a week
Surgical Treatment
Let's talk about surgical treatment
While the NHS can be brilliant, we know it's stressful to have to wait for an operation. So, if there's a wait of longer than 5 weeks on the NHS, you can request access to selected surgical treatments.
Sometimes an operation is the best option – from fixing a hernia and sorting out troublesome tonsils to sorting out unwelcome kidney stones.
The waiting times on the NHS for even minor operations can be lengthy, with delays sadly quite common.
That’s why, if you’re facing a wait of more than 5 weeks for surgical treatment and you've been a member with us for over 6 months*, you can ask for help with over 250 selected surgeries. If we’re able to approve it, we’ll give you the information to help you make your appointments, and we’ll cover the costs directly with the authorised consultant and hospital.
* Unless you joined after 19 February 2024 while living in Northern Ireland – then it's 24 months.
How we can help
If there's a wait for your surgical treatment on the NHS and you've got a report from your consultant for an operation we can help with, you can ask for our help covering the cost of private surgical treatment. (And that includes all the costs involved, such as fees for staff and accommodation.)
You can see the full list of the operations we can cover, but here's a quick overview of the types of surgical treatment we can support:
Orthopaedic (bones, tendons, muscles and nerves)
Urology (urinary organs, like kidneys, and the bladder)
Gynaecology (women's reproductive health)
Ophthalmology (your eyes)
Ear, nose and throat
General surgery (which covers a lot of things that don’t fall into one of the categories above)
Once it's approved, we’ll give you all the info you need, then help you arrange the operation in one of the approved hospitals in our partner network.
"Staff at Benenden Health were kind, helpful and always listened to any concerns I had when arranging my surgical treatment. Three months after my procedure in hospital, I am feeling so much better now."
Jennifer, July 2025
What's not included
Like all the services included in our healthcare, surgical treatments are paid for by our membership fees. So, we make sure the ones we choose are the best possible value and can help as many members as possible.
A few examples of things we don't cover: brain, heart and cancer, which the NHS already does well. Cosmetic surgery, joint replacements and varicose veins.
We'll only ever cover a surgical treatment if it's on our approved procedures list – and we sometimes change the list to make sure we're always offering our members the best value.
Affordable private healthcare
We're not a health insurance provider. We're a not-for-profit who complement the NHS, and we're on a mission to make private healthcare accessible to all.
- No age limits.
- Everyone is accepted (all UK residents).
- No quotes, hidden fees, or excess to pay.
- No medical questionnaire required.
Only £15.85 per person, per month.

How to access Surgical Treatment
You'll need to have seen a consultant and been given a diagnosis of your condition before requesting surgical treatment. You can check you're eligible to access treatment either in the Benenden Health App or in MyBenenden.
Available after 6 months of membership (or 24 months for Northern Ireland^)
-
Referral
Before contacting us, please check you have:
The treatment you've been referred for.
The CCSD code.
Verbal confirmation that the NHS wait time is longer than 5 weeks.
Your consultant's report.
-
Contact us
Once you have all the information ready, you can:
Use the Benenden Health App or
Call our Member Services team on 0300 304 5700 (8am – 5pm Mon – Fri)
-
Requesting treatment
Using the app:
Select Diagnostics and Surgical Treatment from the home screen to submit your request, which will include uploading a copy of your consultant report.
Calling Member Services:
Our advisor will ask for all the information above and a copy of your consultant report.
We'll then review your request and let you know if it's approved.
-
Authorisation
Once your request has been approved, we'll:
Provide you with authorisation to make your appointments with the authorised consultant and hospital.
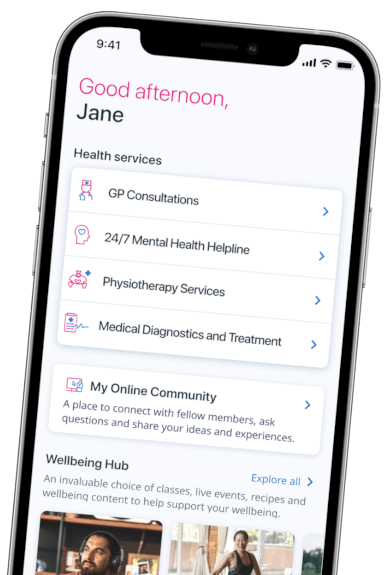
Access via the Benenden Health App
-
Did you know you can start your request for Surgical Treatment through the app.
Simply choose 'Medical Diagnostics and Treatment' and follow the instructions.
Enjoy all your membership benefits on the go:
- Book a telephone or video consultation with a GP in just a few clicks.
- Easily request support via the 24/7 Mental Health Helpline
- Explore the Wellbeing Hub for videos, articles and classes for mental wellbeing, fitness and nutritional health.
- Access rewards and discounts.
-
^ If you're a resident in England, Wales or Scotland when joining you can request Surgical Treatment after six months of membership. If you're a resident in Northern Ireland and joined us before 19 February 2024, you can request Surgical Treatment after six months of membership. If you joined us on or after then you can request Surgical Treatment after 24 months of membership.
Calls to 03 numbers from UK landlines and mobiles cost no more than a national rate call to 01 or 02 numbers. If you receive inclusive free calls to 01 or 02 numbers with your landline or mobile tariff, calls to 03 numbers will also be included.